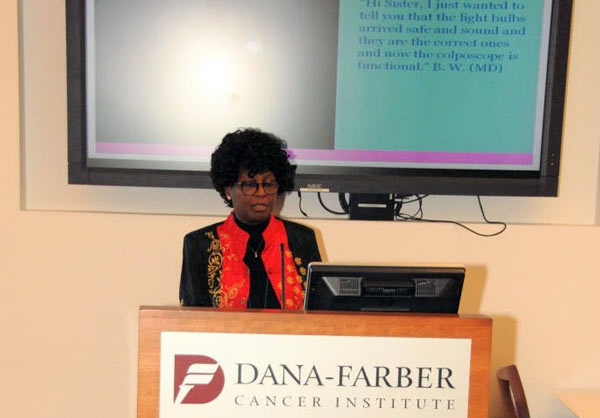
Part of a series of Live Interviews conducted during Global Health Catalyst Cancer Summit, Boston
After putting up a fierce battle with Cancer that included several long and expensive out-of-country trips to far away South Africa, Esther Ikiara lost her husband in May of 2003. What she did next with her anguish and devastation is what ultimately brought her to the Dana Farber Cancer Institute at the Harvard in Boston, Massachusetts for the Global Health Catalyst Cancer Summit. Building on the trappings of their family frustrations, as well as the difficulties to access and afford cancer care for the vast majority of Kenyan patients, she has embarked on a gigantic and ambitious project to build a not-for-profit cancer center in Mombasa, Kenya. The 3.3 Million USD project is more than overdue in a part of the world where it is more likely for a person to be diagnosed and die from cancer than HIV/AIDS. In the course of the next four weeks, DUNIA Magazine will be sharing more interviews of participants – including a provider, a patient practitioner and an advocate – from the Global Health Catalyst Cancer Summit that held at the end of April (29th-30th) at the Harvard Medical School.

DUNIA Magazine: Thank you, Mrs Ikiera for granting us this interview at the 2016 Global Health Catalyst Cancer Summit in Boston, MA. You are a guest all the way from Mombasa, Kenya in Africa. It is a long distance to travel and I wonder the significance and importance of the Summit for you?
Mrs Ikiara: I came to this summit on invitation with the Win-Win team who are my close partners. And I believe that in this Summit I will be able to build partnerships to achieve the project I am trying to do in Mombasa, which is to provide accessibility and affordability of cancer treatment and management as a whole in this part of the world where there are a lot of challenges in getting this treatment.
Could you provide some details with regards to the challenges of accessibility and affordability for patients and their families in this part of Kenya that you are from?
Mrs Ikiara: Yes. The first huge challenge is economical in this part of the world, as a developing country. People have less income. As we all know, the disease, cancer itself is quite costly to manage, even as far as detection because the health seeking behavior of our people is very poor. And so, most of the time they present in late stages, and it becomes very expensive and difficult to manage it at that point, even if you have the access.
So we want to start from education, awareness, early screening and detection and be able to even have a successful rate of reducing the mortality rate.
You talk about these issues with a lot of ease and even a degree of expertise…What is your story and involvement? How did you come into this, knowing that you are not a medical doctor or health practitioner?
Mrs Ikiara: OK…To start with, I have been through the issue myself through my late husband. And from that I developed a lot of interest and got a lot of knowledge about it. I think sometimes you’ve got to go through something to understand it better. From my experience and that of others, now that I’ve gotten involved in and running an outpatient facility, I can tell you for sure that I have learned a lot through these because each time we have to evacuate a patient from our region or any other part, trying to take them to facilities that they can be able to be treated. But unfortunately, it is almost always too late for these. So, from my experience I can say I have learned a lot and this has put me in a position where I engage a lot of these doctors to understand more about cancer.
In an earlier conversation that we were having, you did mention the fact that arcane point in time and because of your outpatient cancer center, you may have come across a gentleman who informed about a potential for a dramatic increase in the incidence of cancer in a certain part of Kenya related to some questionable mosquito nets. Can you talk to us about what you know and what the population needs to be acting on?
Mrs Ikiara: In this particular part of Kenya there is heavy poverty, and it is in the North Eastern part of Kenya where there is very little development, if any. In this area, generally, the water is a problem, as are the sources of water and food. There have been stories that were run in our media, and we have had one-on-one conversations with a couple of doctors regarding the issue of cancer… It came out at as an expose about what was previously deposited there. There is radioactive material in that area. So we are having increased incidences of throat cancer, esophagus and stomach cancers in that area.
This has really not been worked on, but we need to look for ways and means. As you may know, it usually requires a lot of bureaucracy to get through to find out how to penetrate such areas. As of now, that’s the information that I have. But there are so many patients that need help. For us, from my side, we need to engage more as we penetrate and have more collaboration and build partnerships to tackle this issue and get to the bottom of it.
Is there readily available public information about what exactly was deposited?
Mrs Ikiara: According to what the media aired and from discussions I’ve had, it was radioactive material which was never disclosed because the media could not confirm, until there are forensic experts to talk about it. But it has not been brought out. And that’s why I am saying there is a lot that needs to be unearthed in this particular incident.
Finally, now that you are here and we are rounding off this two-day forum, what is your takeaway? Are you satisfied with the meetings and have you had some potential leads for the big and ambitious project presented to the assembly yesterday, that so many, many that will depend on it?
Mrs Ikiara: Yeah…I must say I am a step ahead because currently I have a donor for the radiotherapy machine, so that is a positive aspect of this. I have the Win-Win team (initiative aimed at increasing affordability of cost effective, resource sparing cancer treatment and more important to get better value cancer control and care for patients in the world via exploring scientific approaches and win-win scenarios) who are ready to work with me and who have been guiding me in coming up with different aspects of what needs to be done. So, having those two partners is key, and from the discussions I have had from the conference yesterday and today, I an building up more partnerships. We are looking at ways and means to tackle the different aspects of setting up this (Cancer) facility … my big aim being to build up to an establishment costs which I talked about yesterday totaling to about $3.3 million USD. My hope in this, and I see it probably happening, is that we will connect with people with philanthropic minds to be able to participate in this. Because, if we do a commercial venture, then it will be one of many that are just costly and will not achieve the purposes which I’m here for. So I’m hoping that by the end of this conference I’ll be able to at least leverage some good, positive steps. As I have said, I have already made two major steps. The other step is for establishment costs which I am seeking and I am hoping that I will get some good partners in that.
DM – Thank you so much.
To learn more about the Mombasa Cancer Care Center and the work of Ms Esther Ikiara, visit www.nyalihealthcare.net
Innocent is on Twitter: @InnoChia
Related
– Transforming Cancer Care in Tanzania (using a replicable model) – An Interview with Dr. Twalib Ngoma
– Personalization of problems as a potent antidote in fight against cancer?
– Tiny Drones to Target Cancer: Vote Dr. Wilfred Ngwa to help Cure Cancer – interview
Join mailing list for updates and monthly newsletters