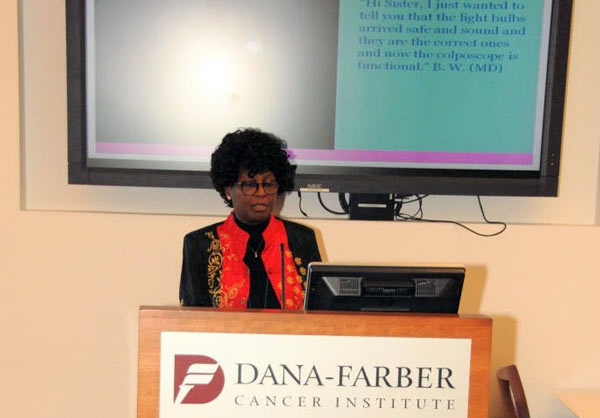
Part of a series of Live Interviews conducted during Global Health Catalyst Cancer Summit at Harvard in Boston
There is no denying the fact that at a forum with cancer as the subject, the expectation is hardly for idle giggling. Yet, the soulful, radiant and beautiful Liz Omondi, a dazzling Kenyan who works and lives in New York City with a rare type of cancer that has taken her body captive, remains undaunted and fights back with an attitude of defiant hope and humor.
At the Global Health Catalyst Cancer Summit last April in Boston, and as she shares in this exclusive with DUNIA, she is not going to give up on herself or on her doctor and his team that have been working marvels. Neither should anyone give up, no matter what your situation is. Liz Omondi’s selfless goal is to build a reliable database of every oncologist in Africa. Read on…

DUNIA Magazine: Thank you, Ms Omondi, for making the time to talk with DUNIA Magazine at this Global Health Catalyst Cancer Summit at the Harvard Medical School in Boston. I have just been inspired by so much over the last couple of days. I couldn’t help but notice a couple of people wipe off a tear or two while you were doing your presentation….because you were talking so positively and bubbling with energy …in spite of your own condition. You have CLL. I bet many of us outside the confines of this room of cancer specialists and advocates and survivors, don’t know what it means. I know I did not. Talk to me about CLL and how you got to this point at this young age?
Ms. Liz Omondi: Thank you Innocent for this opportunity to interview and also thank you to DUNIA Magazine for coming to cover the event. We really need more coverage to create awareness about cancer, more specifically in Africans especially those living here in the US as members of the diaspora, and also the global community as a whole.
I am Elizabeth Omondi. I am from Kenya. I came to the US as a student and I have been living here since and working in New York City. I was diagnosed in 2011.
My story is a rare one. Most people with cancer always are diagnosed accidentally, if I can call it that. A lot of people may be having the disease but it never reveals itself visibly. In oncology language they call it indolent. Cancers like that are slow growing… they are not very aggressive.
So, mine is Chronic Lymphocytic Leukemia, (CLL). It is a type of non-Hodgkin’s lymphoma. It is predominantly common in male Caucasians, median age of 62. My diagnosis came as a surprise to so many – oncologists, pathologists, and other physicians as well who are familiar with CLL – because of my race and age.
At the time of diagnosis I was 32 (so that gives you my age), I am an African woman – very rare. In the Cancer practice of my Oncologist who is based at New York Weill Presbyterian College in New York, I am the only African woman, Black person with this condition at this age.
Most of his patient population are male and female Caucasians, between ages 50s to 60s. His youngest patient was a pediatric boy who was at the time 18, 19 years old. That’s his youngest patient that I am aware of. But that again is a rare one, just like myself being with this disease.
I am also actually a human subject. I offered to be part of it even though he ended up asking me later on.
What does it mean to be a human subject?
Liz Omondi: To be a human subject for research is to participate in research to better understand the disease. So, as I did mention in the talk, Chronic Lymphocytic Leukemia (CLL) is what you call an idiopathic disease. Those are diseases whose causes we do not know. The risks are mentioned, but we cannot say conclusively that these are the risks that are associated to the disease. So we really don’t know what causes it. So there is a lot of research taking place at that end.
And once you better understand the cause and the risks, that’s when you can better come up with a cure. Most of the treatment we currently have, which has been really successful compared to other cancers, is more therapeutic. It buys you more time. Granted, most people will not be able to have normal lives – meaning that they tend to be very tired; you’re going to have symptoms which make you not be as active as you were every day. But it buys you time. I can call it “a lease of life” to you as a patient. So those are some of the successes of CLL.
Many patients, again being that they are older, usually also have another host of diseases that come with aging. And being that they are comorbidities, your body can no longer handle the strong drugs. The drugs are really, really strong. For me, one of the key advantages has been age. The drugs also have adverse side effects, which can be often painful. Where morphine doesn’t work it is excruciatingly painful. In many incidents many of the older patients end up choosing end of life versus going on therapy because, you know, it is too much. You know, quality of life does matter. And so most choose to die a peaceful death. I do understand.
If you asked me this, let’s say five (5), ten (10) years ago, I would have been fighting for their lives. I would have been like “there is no need to kill yourself”. But having lived with this disease, and gone through treatment, and experienced the adverse side effects and just the symptoms of the disease, you kind of see how someone comes to that conclusion. It’s normally not the best, I guess. But for me I think if I were in their bodies I would most likely choose that option as well. Anyway, to each their own. We cross the bridge when we arrive it. We make the decisions then.
The other condition I do have is Red Cell Aplasia. That’s another rare condition, an extremely rare condition. It’s a blood disorder. It is a disease of the bone marrow. I am not making blood. There is something in my immune system killing my blood cells. So, I am also taking medication to address that. Currently, actually, the Red Cell Aplasia is what is giving my doctor more stress and creating more concerns than the cancer.
The reality is that when people hear ‘cancer’, they are more familiar with cancer and so they will react to the cancer. But Oncologists in the room know clearly that Red Cell Aplasia is actually worse than the CLL in terms of hierarchy. So this is concerning, in terms of what is keeping my doctor active and on his toes. And he’s doing an amazing job.
It is not an easy disease. As I say, medicine, I have come to learn is like farming. There is no black and white. You train on how to engage and intervene on caring for a patient. But, it’s up to you, once you have a patient, to come up with a formula. It might work, it might not work. Another oncologist may have a different formula. The oncologist I had before my current one, used a completely different treatment plan that required a lot of chemo. And when I went to my current one he was of the view “let’s avoid chemo and bone marrow transplant” because chemo has many side effects; many healthy organs get destroyed and he was trying to preserve those organs as well as my stem cells.
There is a lot of research going on within the Leukemia/Lymphoma space. Who knows, this research may yield better treatment or even a cure. As one of the human subjects, I hope possibly that they find from this Kenyan what the cause of CLL is. Wouldn’t that be good news for Africa … (rapturous laughter).
Yes indeed! One thing about you that thankfully cannot possibly be contained is your positive energy. How important is a positive attitude for the healing process?
Liz Omondi: So, when I was diagnosed, it’s interesting. You are given these lovely folders to help you figure out so many things that you don’t think about much. One of the things they also offered was a psychiatrist…
And as an African I know Africans don’t like psychiatrists…
Liz Omondi: ….and I am like “why in hell…” – OK, pardon the profanity – “why on earth am I talking to a psychiatrist? I am not sad and I am not upset.” When I was told I had the disease, I remember I was in the exam room and the Oncologist told me I had lymphoma and he was panicking. He looked really concerned. He was a really good oncologist. He was like, “you know what lymphoma is”? I said, “Yes. I know what lymphoma is.” He said “You know it’s cancer?” I replied, “Yes, I know it is cancer.” He said “It’s OK. You can cry Elizabeth. My wife cries, my kids cry in front of me. Just cry. Just let yourself”.
And I am like “maybe I need to pinch myself so I can cry because I don’t feel like crying”. And he’s like “no, just cry if you feel like crying”.
In life I have a rule, if I do not have control over the outcome, no matter what I do in-between will yield no change. I have no control. So if I cry or I scream, for me, it doesn’t make sense. I will cry over something I feel I can impact to change, something I’m confident will yield some results. But If I have no control over this disease, my doctors don’t know what outcome to expect because of the rare combination of the disease, my age, and the Red Cell Aplasia, including another condition I didn’t mention – Alpha thalassemia trait – there’s no point in being sad about it.
The other thing also is that, one of the advantages, if I can call it so, of knowing I have this disease is that it made me look at life through a different lens…in terms of setting goals about life. I think we live like we are going to be here for another sixty (60) years. I don’t take living for granted anymore. I set much more realistic goals. I have a bucket list which has been revised and now it is more efficient and looks real.
What’s on that bucket list?
Liz Omondi: Oh, one of them was to go to Fiji….lol…then I had to delete it. That’s when Cancer Africa came in because I felt Fiji is about me, whereas I need to give back to the continent. One day I was pondering on my experience and was looking up information about cancer in Africa because I wanted to go back home, to spend more time with family. When I was told about lymphoma, I didn’t know much about it. My assumption was that I didn’t have long to live. So I was trying to figure out what resources we have at home – which doctors that I could go talk to, who would be my care provider. And then I found out we didn’t have an accessible, reliable database. That’s what led to the creation of Cancer Africa.
So Cancer Africa is a resource tool where anybody can go on to the website and search – like a Google Search tool – for providers in Africa. Is that correct?
Liz Omondi: Yes, it is a program that is still under development. When I initiated it, I thought it was going to be the easiest project ever because we don’t have many cancer doctors and many countries have none. But I think the strategy I used has made it much slower. Which is, contrary to other projects where we just have a laundry list of people, I am doing some fact-finding and due diligence in terms of making sure that those who claim to be oncologists are indeed oncologists and trained as such.
Are you saying there are some who are practicing in Africa who are really not Oncologists? How possible is that?
Liz Omondi: Yeah. So, what happens is that we have people come to the US, Asia or travel to other developed countries on what we call observerships – where basically you are watching and seeing what’s happening with patients, but you are not interacting, you are not providing any care, you are not doing any operations. At the end you get a certificate of fellowship or observership. It is very common all over the world.
What alarmed me was once when I was watching the news station in Kenya and this fellow came on to be interviewed on gynecological cancers – like Cervical cancer and the likes. And he was introduced as an oncologist. I had gone through the entire Licensing Board’s list of doctors in Kenya and I had the names of all licensed oncologists. So I went to look into his resume, and found that he had travelled to the US, I think it was at the University of Maryland, where he did a clerkship. He is not an oncologist. Yes he is a physician, he is a medical internist as you will call them in the US. But he is not sub-specialized, trained specifically in oncology.
That being said, I understand the resource deficiency in Africa. We don’t have many sub-specialists, but to go out and profess to be a sub-specialist in something (that you are not) is a misrepresentation in my point of view.
I feel like once we have a clear and reliable database, it will then give us the knowledge base on how to shape and design policy. What is our deficiency status? If we have only one oncologist like in Rwanda (who practices at the military hospital), then let’s take stock of what we have. How can we engage to improve the human resource capacity? We may need to be innovative because you are not going to train twenty (20) specialists overnight. So what happens?
Once you have true information it’s easier that way to come up with solutions that are pragmatic, that are enduring. Otherwise you are just going round and round in circles. You are going nowhere, unfortunately.
Thank you so much for this time, Liz.
Liz Omondi: Thank you so much Innocent. And DUNIA should keep coming to these events.
The Cancer Africa website is not yet available. We will share it with you as soon as information becomes available.
Innocent is on Twitter: @InnoChia
Also in DUNIA Mag’s Cancer Series
– Transforming Cancer Care in Tanzania (using a replicable model) – Interview with Dr. Twalib Ngoma
– On Cancer Care in Kenya … An interview with Esther Ikiara
– Personalization of problems as a potent antidote in fight against cancer?
Join mailing list for updates and monthly newsletters